|
Our MACRA Programs
Organizations
|
|
A Proven Healthcare Cost Containment Solution
CUHSM.ORG
is committed to helping our nation achieve better and affordable care,
and improving the overall health of Americans. It is thought that between a third and a half of all medicines prescribed for long term conditions are not taken as recommended. If the prescription is appropriate, then this may represent a loss to patients, the healthcare system and society. The costs are both personal and economic. Adherence presumes an agreement between prescriber and patient about the prescriber's recommendations.
Adherence to medicines is defined as
the extent to which the patient's action matches the agreed
recommendations. Non-adherence may limit the benefits of medicines,
resulting in lack of improvement, or deterioration, in health. The
economic costs are not limited to wasted medicines but also include the
knock˗on costs arising from increased demands for healthcare if health
deteriorates. Non-adherence should not be seen as the patient's problem. It represents a fundamental limitation in the delivery of healthcare, often because of a failure to fully agree the prescription in the first place or to identify and provide the support that patients need later on. Patient adherence has grown to epidemic proportions.
Choosing to include our patient adherence metrics coupled with our integrated CMS submission process saves your organization time, effort and resources. Specifically,
CUHSM.ORG
analyzes the implementation issues and administers solutions for the
Healthcare Delivery problem of Patient Adherence: |
 |
Patient follow-up enhances adherence
|
|
|
|
Patient Adherence Metrics
|
|
|
|
Patient Adherence Communications
|
|
|
Personalized Attention
1. Schedule |
|
|
 |
Our Adherence Roadmap integrates with your business practices
|
|
|
IN DEPTH RESEARCH FOCUS ON SPECIALTIES PATIENT ADHERENCE METHODOLGIES AND METRICS |
Examples of Patient Adherence methodologies for specialties: FAMILY PRACTICE - Reasons for Nonadherence to Medications (HealthDay News) — Eight reasons associated with patient's intentional nonadherence to medications have been identified in a report published by the American Medical Association (AMA). Noting that data show about one-quarter of new prescriptions are never filled, and that about 50 percent of the time patients do not take their medications, the report discusses reasons for intentional nonadherence. According to the report, fear of potential side effects is one main reason for intentional nonadherence. In addition, cost may affect whether patients fill their prescriptions or ration their medication supply. Misunderstanding the need for medication, the nature of side effects, and the time taken to see results also affects nonadherence. Other factors that impact nonadherence include having too many medications, lack of symptoms, concerns about becoming dependent on medications, and depression. Mistrust of the doctor's motivations behind prescription of certain medications also influences nonadherence. "A free online module can help you address these reasons and improve medication adherence in your practice," according to the article. "The module, part of the AMA's STEPS Forward collection, includes practical strategies and tools that you can immediately implement with your practice team." 8 reasons patients don't take their medicationsMedication nonadherence—when patients don’t take their medications as prescribed—is unfortunately fairly common, especially among patients with chronic disease. Learn eight reasons why patients don’t take their medications and ways your team can help identify and improve patients’ adherence to their medications. Patients can be reluctant to tell you that they don’t take their medicines. If you don’t have a true picture of a patient’s medication-taking behavior, you may needlessly escalate his or her treatment, resulting in potential harm to the patient, unnecessary work for the practice and increased costs overall. Data show about one-quarter of new prescriptions are never filled, and patients do not take their medications about 50 percent of the time. Most nonadherence is intentional—patients make a rational decision not to take their medicine based on their knowledge, experience and beliefs. The top eight reasons for intentional nonadherence are:
---------------------------------------------
CardioVascular: Reasons patients give for not following regimen
9 Nonadherence
was an active decision, misunderstandings of
the condition ,General disapproval ,medication, facilitate daily life
or, minimize adverse effects.
Non-Adherent patients gave less evidence of
involvement. -------------------------------------------
Antiretroviral: Reasons
for HAART adherence Abstract The objective of the study was to define common reasons for non-adherence (NA) to highly active antiretroviral therapy (HAART) and the number of reasons reported by non-adherent individuals. A confidential questionnaire was administered to HIV-seropositive patients taking proteinase inhibitor based HAART. Median self-reported adherence was 95% (n = 178, range = 60-100%). The most frequent reasons for at least 'sometimes' missing a dose were eating a meal at the wrong time (38.2%), oversleeping (36.3%), forgetting (35.0%) and being in a social situation (30.5%). The mean number of reasons occurring at least 'sometimes' was 3.2; 20% of patients gave six or more reasons; those reporting the lowest adherence reported a significantly greater numbers of reasons (p = - 0.59; p < 0.001). Three factors were derived from the data by principal component analysis reflecting 'negative experiences of HAART', 'having a low priority for taking medication' and 'unintentionally missing doses', accounting for 53.8% of the variance. On multivariate analysis only the latter two factors were significantly related to NA (odds ratios 0.845 and 0.849, respectively). There was a wide spectrum of reasons for NA in our population. The number of reasons in an individual increased as adherence became less. A variety of modalities individualized for each patient are required to support patients with the lowest adherence. ----------------------------------------------------------------- MENTAL
HEALTH SPECIALTIES:
|
|
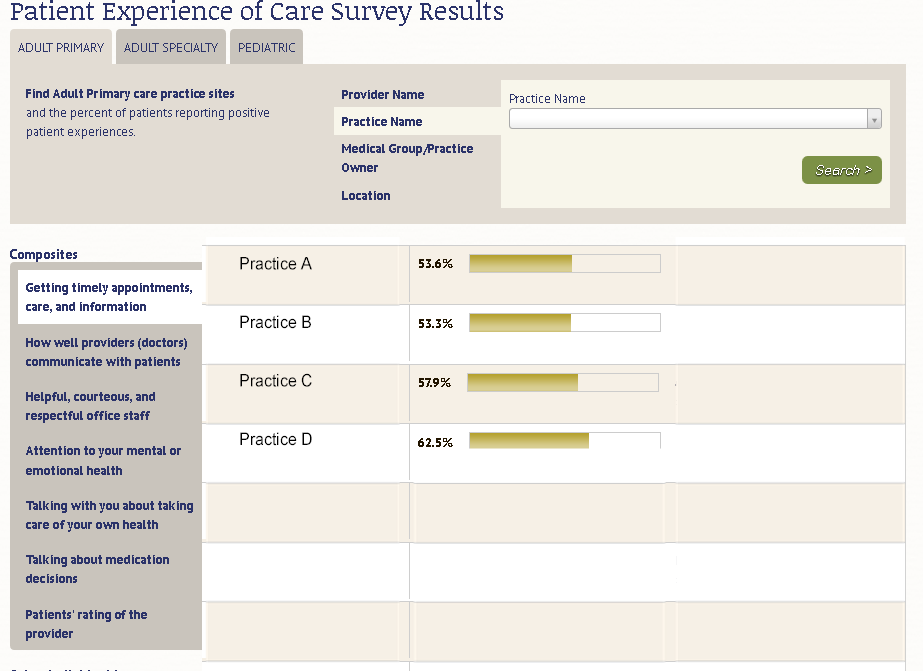
By measuring patient experience, health care providers can identify areas for improvement to engage patients to make informed choices concerning regimen compliance in association with health care providers and services. See the representative Survey results below.
To research how Patient Experience websites can be designed to
|